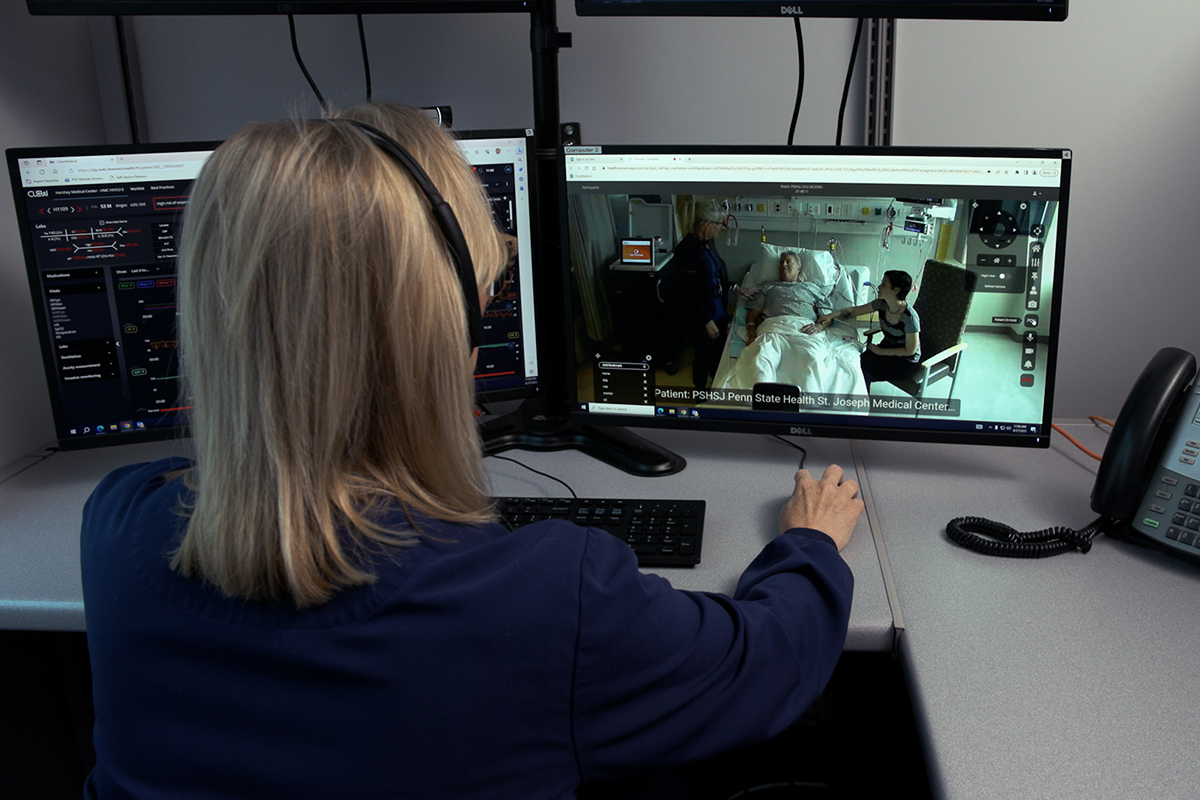
 Mimi Beck, a registered nurse in the Critical Care Unit at Penn State Health St. Joseph Medical Center, speaks with Susan Richwine, registered nurse care manager – Virtual Intensive Care Unit at Penn State Health, via video conferencing from a patient’s room.
Mimi Beck, a registered nurse in the Critical Care Unit at Penn State Health St. Joseph Medical Center, speaks with Susan Richwine, registered nurse care manager – Virtual Intensive Care Unit at Penn State Health, via video conferencing from a patient’s room.
The patient was critically ill from an overdose of Tylenol. Monitoring the patient remotely with high-resolution cameras, microphones and electronic medical devices, a virtual critical care physician was immediately concerned about potential liver damage and quickly sought emergency consultation from nephrology and vascular services.
December 5, 2023
Several days later, the patient was discharged from Penn State Health St. Joseph Medical Center in Reading with no liver damage. “Virtual ICU services were right there on hand to provide that immediate evaluation, facilitating lifesaving treatment,” said Andrea Ryan, nurse manager in the medical center’s Critical Care Unit.
Successful patient outcomes like this give special meaning to the one-year anniversary of Penn State Health’s virtual intensive care services, whose intensivists, specially trained critical care nurses and other clinicians supplement care provided in person by bedside staff. The vICU became an internal service following a more than six-year external partnership.
Creating a unified operation
“Our goal from the beginning was to support our critical care mission and respond to the unique needs of the ICU patient,” said Chris LaCoe, vice president for Penn State Health Virtual Health. “Our initial partnership enabled Penn State Health to develop competencies in providing virtual intensive care and gain additional clinical expertise and experience in providing these services.”
A unified, internal operation is important, added Dr. Will Hazard, director of virtual intensive care. “When we appear on the audio-video system to both bedside staff and the patient, we are Penn State Health. Process improvement, accountability and institutional protocols all flow through the greater health system, and we are able to tailor our support based on the individual hospital and even to the individual unit.”
That support encompasses extensive experience. “Over 20 specially trained virtual ICU nurses who bring more than 400 years of experience to their care, work 24/7 to support the beside teams,” Kelly Hollenbeak, supervisor of virtual care nursing, said.
Virtual services are aimed at leveraging technologies to support delivery of care and patient monitoring, while freeing bedside staff members for additional direct care with more patients. “Our bedside staff do an outstanding job caring for patients, and virtual care is focused on how we support bedside nurses and provide resources to reduce burnout while improving patient safety. We help with documentation, monitor frequent vital signs, provide medication reviews and provide complete critical care consultation and monitoring,” LaCoe said.
Virtual care counters projected nursing shortage
In addition, virtual care can help to address labor market concerns, including a projected shortage of 200,000 to 450,000 nurses by 2025, Hazard said. “It also can provide an avenue for individuals who want to continue to work in positions such as nursing but may have physical limitations or family care obligations that prevent them from the demands of in-person clinical duties.”
In the past year alone, virtual care at Penn State Health expanded from its base of board-certified critical care physicians and critical care nursing services to include respiratory therapy and emergency room care. Virtual intensive care services are provided at Penn State Health Milton S. Hershey Medical Center, Penn State Health Lancaster Medical Center and St. Joseph Medical Center. Virtual emergency room services were added in mid-July at the Milton S. Hershey Medical Center.
Penn State Health Hampden and Holy Spirit medical centers are being evaluated for potential expansion of vICU services, LaCoe said. The addition of virtual pharmacy services also is being considered.
Artificial intelligence to help guide decisions
As the virtual-technology platform continues to evolve, LaCoe added, “it will serve as a means to employ the existing labor force more effectively and efficiently by offloading some of the more burdensome aspects of patient care such as assessments, forms and some documentation. It will make patient triage and transfer more efficient, fill gaps in services and staffing, and use existing expertise without costly and potentially disruptive patient transfers.”
The service also is on the verge of more extensively integrating artificial intelligence as a clinical decision-support tool, something “that needs to be explored out of necessity due to workforce shortages and health care’s increasing complexity,” Hazard said.
Sometimes, the virtual ICU enables care over distances greater than within the hospital system. Megan Swope, a virtual ICU RN care manager, was caring for a patient for whom end-of-life decisions needed to be made. “With the help of Samantha Luvison, another virtual ICU RN care manager, we were able to teleconference in family members who were hours away by car or plane.”
Not only did the family members help to make difficult decisions, but they also were able to be present with their family member during the patient’s final moments. “They could be together to support one another and their family member, while also dealing with their grief,” Swope said.
“Virtual critical care is cutting edge. It allows us to interact with our patients in very meaningful and supportive ways,” she added.
